
Understanding how the ketogenic diet interacts with insulin is like discovering the secret handshake of metabolic health.
Mastering the Keto–Insulin Connection: Your High-Energy Roadmap to Fat Burning and Balanced Blood Sugar
- Introduction to Keto and Insulin – Why this metabolic duo matters
- Basics of Insulin Physiology – The hormone behind fat storage and energy use
- What Happens to Insulin on a Standard High-Carb Diet – Roller-coaster glucose explained
- Mechanisms of Ketosis and Insulin Reduction – How very-low-carb eating flips the metabolic switch
- Benefits of Lower Insulin Levels on Metabolic Health – From weight management to brain clarity
- Keto Adaptation Phases and Hormonal Shifts – Timeline of change inside your cells
- Common Misconceptions about Keto and Insulin – Debunking Internet myths
- How to Start Keto Safely with Insulin Sensitivity Issues – Doctor-approved first steps
- Monitoring Biomarkers: Glucose, Ketones, and More – Data-driven self-tracking tips
- Nutrient Timing and Carb Cycling Strategies – Using strategic carbs without spiking insulin
- Dealing with Keto Flu and Blood Sugar Fluctuations – Practical relief tactics
- Special Populations: Diabetics, Athletes, Women – Tailoring keto for unique needs
- Food Choices: Fats, Proteins, and Low-Carb Vegetables – The ultimate grocery checklist
- Lifestyle Factors: Sleep, Stress, Exercise Impact on Insulin – Beyond the plate
- Troubleshooting Plateaus and Reintroducing Carbs – Fine-tuning for long-term success
- Conclusion – Key takeaways and motivation
- FAQs – Five highly Googled questions answered
Mastering the Keto–Insulin Connection: Your High-Energy Roadmap to Fat Burning and Balanced Blood Sugar
Introduction to Keto and Insulin
Understanding how the ketogenic diet interacts with insulin is like discovering the secret handshake of metabolic health. Most of us know insulin only as “the blood-sugar hormone,” but its reach is far wider: it decides whether you torch fat for fuel or squirrel it away for a rainy day. The keto diet—defined by a daily carb intake below roughly 50 grams—flips your primary energy source from glucose to fat-derived ketones. That shift dramatically lowers circulating insulin, creating a biochemical environment where fat loss, steady energy, and craving control thrive. This article unpacks every layer of that connection, giving you science-based tactics plus real-world tips to stay energetic, focused, and lean while keeping blood sugar on an even keel. Ready to dive in? Let’s decode the keto–insulin dance step by step.
Basics of Insulin Physiology
Insulin, produced by the beta cells of your pancreas, acts as a molecular key. After you eat carbs, blood-glucose levels rise, prompting insulin release. Insulin unlocks muscle and liver cells so glucose can flow in and be burned or stored as glycogen. Excess glucose? Insulin signals fat cells to absorb it and convert it to triglycerides. Chronic high-insulin exposure, driven by frequent carb-rich meals or sugary snacks, tells your body “store, don’t burn,” leading to weight gain and, in time, insulin resistance. Imagine insulin as an email notification system; too many pings and your inbox (receptors) start ignoring the messages. The keto diet’s ultra-low carb intake slashes those pings, giving insulin receptors a break and restoring their sensitivity. Over time, your pancreas needn’t pump out as much insulin, and fat cells receive the memo: “Unlock; it’s time to burn.” Grasping this hormonal signaling sets the foundation for why keto can be a metabolic game changer.
What Happens to Insulin on a Standard High-Carb Diet
Picture a typical Western breakfast—cereal, orange juice, maybe a muffin. Carbs flood the bloodstream; insulin spikes to herd glucose into cells. Two hours later, glucose dips, you feel hungry again, and the cycle repeats at lunch and dinner. This roller-coaster leaves insulin elevated most of the day. High insulin inhibits hormone-sensitive lipase, the enzyme responsible for releasing stored fat, so despite having plenty of body-fat calories on hand, you can’t access them. Over time, cells become numb to insulin’s signal—insulin resistance—forcing the pancreas to produce even more. Eventually, this strain can lead to pre-diabetes or type 2 diabetes. The irony? Many people feel tired and hungry even while overeating calories. Recognizing this vicious loop underscores why reducing carbs (and thus insulin) through keto can reset metabolic flexibility, allowing easy access to body-fat stores without constant hunger.
Mechanisms of Ketosis and Insulin Reduction
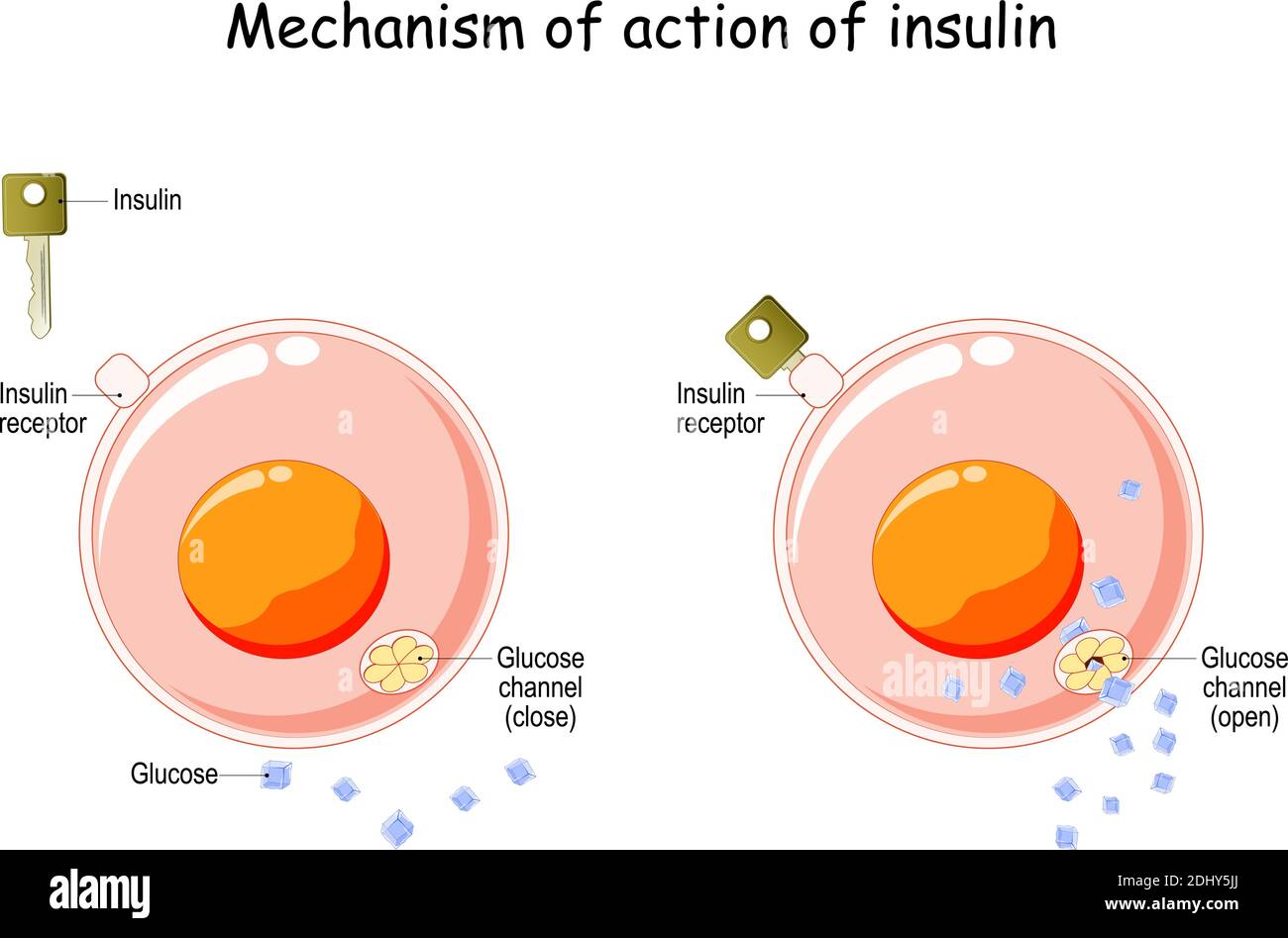
Ketosis begins when dietary carbs drop low enough that liver glycogen (your glucose storage tank) empties. With glucose scarce, insulin levels fall because less is required to manage blood sugar. Low insulin signals adipose tissue to release fatty acids, which travel to the liver and convert into ketone bodies—beta-hydroxybutyrate (BHB), acetoacetate, and acetone. These ketones supply energy to the brain and muscles, sparing protein and maintaining mental clarity. Think of ketones as high-octane fuel produced on-site. Meanwhile, lower insulin unlocks stubborn fat deposits, especially visceral fat around organs. Research shows fasting insulin can drop by up to 50 percent within weeks of a well-formulated ketogenic diet. With insulin downregulated, inflammation markers often fall, HDL (the “good” cholesterol) climbs, and triglycerides plunge. This cascade explains the surge in steady energy and reduced cravings that keto enthusiasts rave about.
Benefits of Lower Insulin Levels on Metabolic Health
Shedding excess insulin offers a buffet of health perks. First, fat oxidation soars, translating into weight loss without calorie obsession. Second, stable insulin improves leptin signaling—the hormone telling your brain you’re full—helping curb overeating. Third, low insulin reduces sodium retention, naturally lowering blood pressure. Studies connect lower fasting insulin with diminished risk of heart disease, certain cancers, and neurodegenerative disorders. On the cognitive front, ketones provide a more efficient fuel source for neurons, enhancing focus and memory. Many keto adopters report fewer afternoon slumps and more even moods, owing to insulin’s influence on neurotransmitter pathways. Athletically, once fully adapted, athletes tap into virtually limitless fat reserves for fuel, delaying glycogen depletion. In short, dialing down insulin via keto is like switching your body from a battery-powered flashlight to a self-recharging LED—brighter, longer-lasting, and more reliable.
Keto Adaptation Phases and Hormonal Shifts
The road to full keto adaptation typically unfolds in four phases over four to eight weeks. Phase 1: Glycogen Depletion (days 1-3) brings quick water and salt loss as glycogen stores empty, dropping insulin sharply. Phase 2: Early Ketosis (days 3-14) introduces mild ketone production; some experience “keto flu” symptoms—fatigue, headaches—largely from electrolyte imbalance. Phase 3: Fat Adaptation (weeks 2-6) sees muscles ramp up enzymes to oxidize fat efficiently; energy levels rebound. Insulin stabilizes at lower levels, and hunger hormones ghrelin and leptin recalibrate. Phase 4: Metabolic Flexibility (weeks 6+) allows seamless switching between fat and ketones, granting steady performance even with sporadic carb intake. Understanding this timeline helps manage expectations and underscores the importance of mineral intake—sodium, potassium, magnesium—to smooth hormonal transitions and keep insulin in its newly reduced groove.
Common Misconceptions about Keto and Insulin
Myth 1: “Keto destroys your thyroid.” Reality: While very-low-carb eating can slightly lower T3 (active thyroid hormone), studies show basal metabolic rate remains stable, likely because ketones themselves increase energy efficiency. Myth 2: “You must eat zero carbs forever.” Actually, many thrive with targeted or cyclical carb intakes once insulin sensitivity improves. Myth 3: “Eating fat raises insulin.” Pure fats like olive oil or butter barely nudge insulin; protein has a modest effect; carbs spark the big surge. Myth 4: “Keto equals unlimited bacon.” A quality ketogenic diet emphasizes whole foods, leafy greens, and healthy fats, not just processed meat. Busting these misconceptions clears mental clutter and helps you focus on what really moderates insulin: carb quantity and quality.
How to Start Keto Safely with Insulin Sensitivity Issues
If you’re insulin-resistant or diabetic, consult your healthcare provider first—medication dosages may need adjusting rapidly. Begin by clearing your pantry of refined carbs: bread, sugary drinks, cereals. Stock up on nutrient-dense fats (avocado, coconut oil), moderate protein (eggs, wild-caught fish), and above-ground vegetables. Transition gradually by reducing carbs over a week to minimize shock. Prioritize hydration—aim for three liters of water daily—and add 2 grams of sodium through broth or mineral salt to offset insulin-driven sodium excretion. Track blood glucose and ketones; many use a dual meter for real-time feedback. Slow, deliberate entry lets your pancreas, liver, and gut microbiome adapt, preventing hypoglycemia and ensuring a smoother insulin downshift.
Monitoring Biomarkers: Glucose, Ketones, and More
Data turns guesses into precision. Check fasting glucose first thing in the morning; optimal ranges often fall between 70-90 mg/dL once keto-adapted. Post-meal glucose should ideally rise less than 30 points. Ketone levels of 0.5-3.0 mmol/L suggest nutritional ketosis. Triglyceride-to-HDL ratio below 2 hints at improved insulin sensitivity. Fasting insulin lab tests (<10 µIU/mL) provide deeper insight. Continuous glucose monitors (CGMs) offer minute-by-minute curves, revealing how specific foods or stressors affect insulin demand. Logging these metrics in an app helps spot patterns, enabling micro-adjustments—like swapping a snack or shifting workout timing—to keep insulin tame and fat-burn flames high.
Nutrient Timing and Carb Cycling Strategies
Once metabolically flexible, some people leverage strategic carb timing—consuming 20-40 grams of complex carbs around intense workouts—to replenish glycogen without major insulin spikes. Others practice a weekly “refeed,” bumping carbs to 100-150 grams from sweet potatoes or berries, which can boost thyroid function and workout performance. The key? Stay keto most days so your insulin baseline remains low. Monitor the next morning’s fasting glucose; if it remains under 95 mg/dL, your carb cycling is likely compatible. Think of insulin like a thermostat—you can allow brief warm-ups (carb intakes) as long as the system cools back down quickly.
Dealing with Keto Flu and Blood Sugar Fluctuations
Keto flu arises from rapid electrolyte shifts as insulin falls. Symptoms include fatigue, dizziness, and irritability. Counter them by drinking salted water, taking magnesium glycinate (300-400 mg nightly), and consuming potassium-rich foods like avocado and leafy greens. If blood sugar dips below 65 mg/dL with shakiness, eat a tablespoon of almond butter; the fat blunts a glucose rise while providing quick relief. Gradual carb reduction and adequate electrolytes ensure insulin adjusts gracefully, preventing dramatic swings.
Special Populations: Diabetics, Athletes, Women
Type 2 diabetics often see dramatic reductions in insulin requirements; however, medical supervision is vital to avoid hypoglycemia. Endurance athletes may experience initial performance dips but rebound stronger once fat-adapted. They may use targeted carbs pre-race without derailing insulin control. Women, especially during luteal phase or pregnancy, may need slightly higher carbs (~50-80 grams) to support hormone balance. Listening to biofeedback—energy, mood, menstrual health—helps fine-tune carb and fat ratios while maintaining overall insulin sensitivity.
Food Choices: Fats, Proteins, and Low-Carb Vegetables
Build meals around fatty fish, pasture-raised eggs, extra-virgin olive oil, and a rainbow of non-starchy veggies. Leafy greens supply potassium and magnesium critical for insulin signaling. Choose grass-fed meats for higher omega-3 content. Limit processed seed oils and watch protein portions—excess protein can convert to glucose via gluconeogenesis, modestly raising insulin. Season with turmeric, cinnamon, and vinegar—spices shown to improve insulin sensitivity. Dessert? Berries with coconut cream satisfy cravings without a carbohydrate bomb.
Lifestyle Factors: Sleep, Stress, Exercise Impact on Insulin
Six hours of poor sleep can reduce insulin sensitivity by 20% the next day. Aim for seven to nine hours in a dark, cool room. Chronic stress elevates cortisol, which in turn raises glucose and insulin. Incorporate daily mindfulness, whether meditation, journaling, or a nature walk. Strength training boosts GLUT-4 transporter activity, allowing muscles to absorb glucose independent of insulin, giving the pancreas a holiday. High-intensity intervals further enhance insulin sensitivity, while steady-state cardio taps stored fat. Integrating these non-diet levers multiplies keto’s insulin-lowering magic.
Troubleshooting Plateaus and Reintroducing Carbs
If weight stalls, audit hidden carbs—sauces, nuts, keto desserts—and track total calorie creep. Increase protein to 1.6 g/kg lean mass to preserve muscle, and experiment with intermittent fasting (e.g., 16:8) to deepen insulin lows. When reintroducing carbs, start with 25-gram increments of root veggies, monitor glucose, and ensure you return to ketosis within 24 hours. If fasting glucose climbs consistently, pull back. Maintaining a flexible, informed approach keeps insulin in the sweet spot for lifelong vitality.
Conclusion
Mastering the keto–insulin connection empowers you to orchestrate fat loss, mental clarity, and metabolic health without hunger or guesswork. By understanding insulin’s pivotal role and leveraging low-carb nutrition, smart monitoring, and supportive lifestyle habits, you transform your body into a fat-burning, energy-efficient powerhouse. Keep experimenting, stay curious, and enjoy the vibrant health that comes from harmonizing diet and hormones.
Read Also; 5 Powerful Ways the Keto Diet Supercharges Your Metabolism Instantly (You’ll Love #3!)
FAQs https://en.wikipedia.org/wiki/FAQ#
Can I follow keto if I’m on insulin medication?
Yes, but work closely with your doctor—insulin doses often drop quickly on keto to avoid hypoglycemia.
How long before insulin levels improve on keto?
Many see measurable drops in fasting insulin within four to six weeks, though individual timelines vary.
Is it necessary to stay under 20 grams of carbs forever?
Not necessarily. Once insulin sensitivity improves, some thrive on 50-100 grams of quality carbs while maintaining metabolic benefits.
Do exogenous ketones help lower insulin?
They raise blood ketone levels but don’t significantly affect insulin. Real dietary carb reduction remains key.
What’s the best time to test blood glucose for insulin insight?
Fasting morning values and one-hour post-meal readings give the clearest picture of insulin demand and sensitivity.



One Comment